In the realm of healthcare, a Letter of Medical Necessity (LMN) serves as a vital tool in advocating for patients’ needs and ensuring they receive appropriate medical care. This document, typically prepared by a healthcare provider, plays a crucial role in justifying the necessity of specific treatments, services, or items for a patient’s health.
By outlining the clinical rationale and reasoning behind a recommended intervention, the LMN seeks to secure insurance coverage or other benefits that are essential for a patient’s well-being. Understanding the significance and process of obtaining an LMN is essential for patients, healthcare providers, and insurance companies to collaborate effectively in the best interest of the patient.
What Is A Letter Of Medical Necessity?
A Letter of Medical Necessity, often abbreviated as LMN, is a formal document that articulates why a particular treatment, service, or item is medically necessary for a patient’s health. This document is typically written by a healthcare provider, such as a physician, specialist, or therapist, and is used to justify the need for the recommended intervention.
The LMN contains detailed information about the patient’s medical condition, the proposed treatment or service, and the expected outcomes. It acts as a persuasive tool to demonstrate to insurance companies or other relevant parties the clinical reasoning behind the prescribed intervention.
What Is The Purpose Of A Letter Of Medical Necessity?
The primary purpose of a Letter of Medical Necessity is to provide a comprehensive explanation of why a specific treatment, service, or item is essential for a patient’s health. This document helps to justify the medical necessity of the recommended intervention, especially when it comes to insurance coverage or reimbursement. By outlining the clinical reasoning behind the prescribed treatment, the LMN ensures that patients receive the care they need based on their unique medical needs.
1. Advocating for Patients
One of the key purposes of an LMN is to advocate for patients and ensure they receive the necessary treatments, services, or items for their health. The LMN serves as a formal document that articulates the medical necessity of a prescribed intervention, helping to secure insurance coverage or other benefits that are crucial for the patient’s well-being.
2. Ensuring Access to Care
In many healthcare settings, access to certain treatments or services may be contingent upon the approval of insurance providers or other benefit organizations. A Letter of Medical Necessity helps to ensure that patients have access to the care they need by providing a clear justification for the recommended intervention. This document acts as a gateway to essential treatments and services that can significantly impact a patient’s health outcomes.
3. Promoting Patient-Centered Care
By emphasizing the medical necessity of a prescribed intervention, an LMN promotes patient-centered care that is tailored to meet the individual needs of each patient. The document highlights the specific reasons why a particular treatment or service is crucial for managing or treating a diagnosed medical condition, ensuring that patient care remains at the forefront of decision-making.
4. Enhancing Communication
Effective communication is essential in healthcare to ensure that all stakeholders are aligned in the patient’s care plan. A Letter of Medical Necessity serves as a communication tool that facilitates clear and concise messaging about the medical necessity of the recommended intervention. This document promotes transparency and collaboration among healthcare providers, patients, and insurance companies, fostering a shared understanding of the treatment rationale.
5. Guiding Treatment Decisions
Healthcare providers rely on clinical guidelines and evidence-based practices to make informed treatment decisions. An LMN provides additional support for these decisions by articulating the medical necessity of a recommended intervention. By outlining the clinical reasoning behind the prescribed treatment, the LMN helps guide healthcare providers in choosing the most appropriate interventions for their patients.
Difference Between A Letter Of Medical Necessity And A Prescription
It is crucial to distinguish between a Letter of Medical Necessity and a prescription, as these documents serve different purposes in the healthcare landscape. While both documents are essential for ensuring patients receive appropriate care, they each play distinct roles in the healthcare process.
1. Purpose and Scope
A prescription is a written order from a healthcare provider authorizing a patient to receive a specific medication or treatment. It outlines the dosage, frequency, and duration of the prescribed intervention. In contrast, a Letter of Medical Necessity provides a detailed explanation of why a particular treatment, service, or item is medically necessary for a patient’s health. The LMN justifies the need for the intervention and seeks approval for its coverage or reimbursement.
2. Documentation Requirements
Prescriptions are typically used to authorize the dispensing of medications by pharmacists and are often required for insurance coverage of prescribed medications. On the other hand, a Letter of Medical Necessity is more comprehensive in nature, providing a detailed rationale and clinical reasoning for a recommended treatment or service. The LMN may be necessary for treatments, services, or items that require additional documentation for approval.
3. Insurance Coverage
While prescriptions are essential for obtaining specific medications, an LMN is crucial for securing insurance coverage or reimbursement for treatments, services, or items that may not be automatically covered. Insurance companies require documentation that proves the medical necessity of a prescribed intervention, which is where the LMN plays a critical role. By outlining the clinical rationale behind the prescribed treatment, the LMN helps to facilitate insurance approval.
4. Patient-Centered Care
Prescriptions focus on the specifics of a medication or treatment plan, dictating the dosage and administration instructions for the patient. In contrast, an LMN emphasizes the medical necessity of the recommended intervention, highlighting why it is essential for managing or treating the patient’s diagnosed medical condition. The LMN promotes patient-centered care by advocating for treatments or services that align with the patient’s unique needs.
5. Approval Process
While prescriptions are typically straightforward in terms of authorization for medications, a Letter of Medical Necessity may require additional steps for approval. The LMN serves as a formal request for coverage or reimbursement, requiring review and approval from insurance companies or other benefit providers. The detailed explanation provided in the LMN helps to justify the medical necessity of the recommended intervention and facilitate the approval process.
What Are Some Items That Require A Letter Of Medical Necessity?
Various items may require a Letter of Medical Necessity to justify their medical necessity and secure insurance coverage or reimbursement. These items span a range of healthcare services, treatments, and equipment that are essential for managing or treating patients’ health conditions.
1. Durable Medical Equipment (DME)
Durable Medical Equipment (DME) refers to items such as wheelchairs, walkers, hospital beds, and nebulizers that are used to aid in daily living activities or manage medical conditions. Some insurance providers may require an LMN to demonstrate the medical necessity of DME for a patient’s health.
2. Prosthetics and Orthotics
Prosthetic limbs, orthopedic braces, and custom-fitted orthotic devices are examples of items that may require a Letter of Medical Necessity. These specialized devices are crucial for individuals with limb loss or musculoskeletal conditions and require justification for insurance coverage.
3. Home Health Services
Home health services, such as skilled nursing care, physical therapy, occupational therapy, and speech therapy, may necessitate an LMN to secure coverage from insurance providers. These services are essential for patients who require ongoing medical care in their homes.
4. Adaptive Equipment
Adaptive equipment, including items such as shower chairs, grab bars, and feeding tubes, may require a Letter of Medical Necessity to demonstrate their essential role in supporting a patient’s health and well-being. These assistive devices are designed to enhance independence and safety for individuals with disabilities or medical conditions.
5. Medical Procedures or Treatments
Certain medical procedures or treatments, such as chemotherapy, radiation therapy, or surgical interventions, may require an LMN to justify their medical necessity. These interventions often involve high costs and risks, making it essential to provide a detailed explanation of why they are crucial for the patient’s health.
6. Specialized Diagnostics
Advanced diagnostic tests or imaging studies, such as MRI scans, CT scans, or genetic testing, may necessitate a Letter of Medical Necessity to validate their use in diagnosing or managing a medical condition. These specialized diagnostics play a critical role in guiding treatment decisions and monitoring patient outcomes.
7. Medications
Certain medications, especially those that are costly or not typically covered by insurance, may require an LMN to explain why they are medically necessary for a patient’s treatment plan. The document outlines the clinical rationale behind the prescription and justifies the need for the specific medication.
When May You Need A Letter Of Medical Necessity?
The need for a Letter of Medical Necessity arises in various situations where a specific treatment, service, or item requires justification for its medical necessity. Understanding when an LMN is necessary can help patients and healthcare providers navigate the healthcare system more effectively and advocate for the care that is essential for the patient’s health.
1. Insurance Coverage
One common scenario where you may need a Letter of Medical Necessity is when seeking insurance coverage for a particular treatment or service. Insurance companies often require documentation that proves the medical necessity of a prescribed intervention before approving coverage. An LMN serves as a formal justification for the recommended treatment, increasing the likelihood of insurance approval.
2. Reimbursement
When seeking reimbursement for out-of-pocket expenses related to a medical intervention, you may need a Letter of Medical Necessity to support your claim. The document outlines the medical necessity of the prescribed treatment or service, making a compelling case for reimbursement from insurance providers or other benefit organizations.
3. Prior Authorization
Prior authorization is a process that requires approval from insurance companies before receiving certain treatments or services. In situations where prior authorization is necessary, a Letter of Medical Necessity can help expedite the approval process by providing a detailed explanation of the medical necessity of the recommended intervention.
4. Appeals Process
If your insurance claim is denied, you may need to appeal the decision and provide additional documentation to support your case. A Letter of Medical Necessity can help strengthen your appeal by outlining the clinical rationale behind the prescribed treatment and demonstrating why it is essential for managing your medical condition.
5. Special Circumstances
In some cases, a treatment, service, or item may not be automatically covered by insurance and require additional justification for approval. A Letter of Medical Necessity can help navigate these special circumstances by providing a comprehensive explanation of why the prescribed intervention is medically necessary for your health.
How To Get A Letter Of Medical Necessity
Obtaining a Letter of Medical Necessity involves a collaborative effort between the patient and their healthcare provider to ensure that the necessary documentation is prepared and submitted for approval. The process of obtaining an LMN may vary depending on the specific treatment, service, or item in question, but generally involves the following steps.
1. Consultation with Healthcare Provider
The first step in obtaining a Letter of Medical Necessity is to discuss your medical needs with your healthcare provider, whether it be your primary care physician, specialist, or therapist. During this consultation, you can express your concerns and explore treatment options that may require an LMN for approval.
2. Clinical Evaluation and Treatment Plan
Following the consultation, your healthcare provider will conduct a clinical evaluation to assess your medical condition and develop a treatment plan that includes the recommended intervention. This treatment plan outlines the specifics of the prescribed intervention and its expected benefits for managing or treating your diagnosed medical condition.
3. Documenting Medical Necessity
Your healthcare provider will document the medical necessity of the recommended intervention in the Letter of Medical Necessity. This document includes detailed information about your medical condition, the proposed treatment or service, and the expected outcomes. The LMN serves as a formal explanation of why the prescribed intervention is essential for your health.
4. Submission to Relevant Parties
Once the LMN is completed, it is submitted to the relevant parties, such as your insurance company or other benefit providers, for review and approval. The document is a formal request for coverage or reimbursement that outlines the medical necessity of the prescribed intervention and makes a compelling case for its approval.
5. Follow-Up and Communication
After submitting the Letter of Medical Necessity, it is essential to follow up with your healthcare provider and the relevant parties to ensure that the document is processed promptly. Effective communication is key to navigating the approval process and advocating for the care that is necessary for your health and well-being.
How Long Is An LMN Valid?
The validity of a Letter of Medical Necessity may vary depending on the specific treatment, service, or item in question, as well as the requirements of the insurance company or other benefit providers. Understanding the validity period of an LMN is essential for ensuring that you receive continuous coverage for the prescribed intervention.
In general, a Letter of Medical Necessity is considered valid for a certain period of time, typically ranging from six months to one year. This validity period may be specified by the insurance company or other benefit providers and may vary based on the nature of the prescribed intervention.
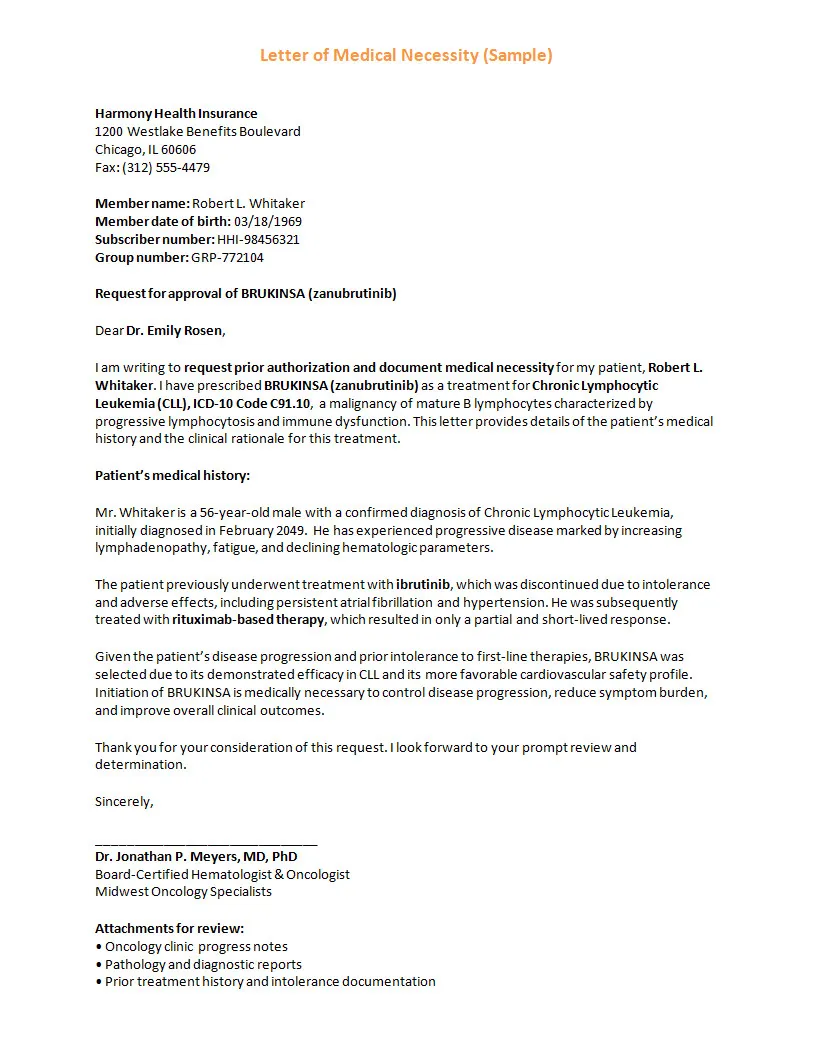
Letter of Medical Necessity Template – DOWNLOAD
- Free Printable Monthly Expenses Template - February 12, 2026
- Printable Monthly Employee Schedule Template - February 11, 2026
- Printable Monthly Budget Planner Template - February 10, 2026